Introduction: Splenic marginal zone lymphoma (SMZL) is a rare B-cell lymphoid malignancy with primary involvement of the white pulp of the spleen. It is a chronic disease, of indolent behavior and with prolonged survival. However, approximately 25% of cases have greater biological aggressiveness, a propensity for histological transformation to high-grade B-cell non-Hodgkin's lymphoma and shortened survival. The recognition of these cases of particular outcome is important for the selection of a risk-adapted therapeutic approach in resource-poor settings.
Methods: In this single-center, retrospective and observational study, we describe the clinical and epidemiological characteristics, analysis of survival, determination of prognostic factors and propose a risk-adapted therapeutic approach, based on data from a cohort of 39 SMZL patients, treated in the largest cancer center in Latin America, from January 1992 to December 2016. Factors with prognostic implications were determined by Cox's univariate analysis, survival curves were estimated by the Kaplan-Meier method and the log-rank test was used to compare curves of survival and to verify the association between categorical variables and survival curves.
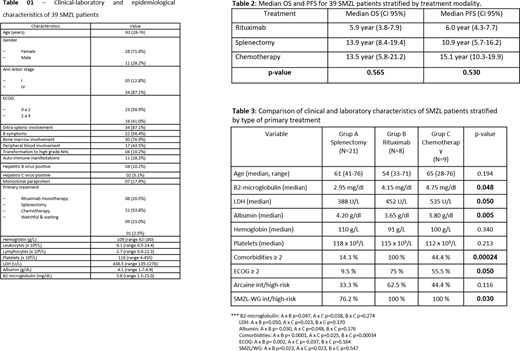
Results: The clinical and epidemiological characteristics of the 39 SMZL patients are summarized inTable 1. There was predominance of female patients (71.8% - 28-29), with a median age of 63 years (28-76) and a higher incidence of B symptoms (56.4% - 22-39) and extra-splenic involvement (87.1% - 34-39) than the results described in series in Europe and North America. With a median follow-up of 8.7 years (0.6-20.2 years), the overall survival (OS) estimated at 5 years and progression-free survival (PFS) were 76.9% and 63.7%, respectively. Factors with an adverse prognostic impact on OS included: LDH ≥ 480 UL (HR: 4.55, 95% CI 1.05-19.70, p = 0.043), albumin < 3.5 g-dl (HR: 7.32, 95% CI 1.46-36.32, p = 0.015), hemoglobin < 100 gL (HR: 4.27, 95% CI 1.01-17.99, p = 0.048), platelets < 100 x 109 (HR: 7.32, 95% CI 2.26-60.54, p = 0.003), high-risk Arcaini score (HR: 14.26, 95% CI 1.65-123.20, p = 0.002) and high-risk SMZL-Working Group score (HR: 6.66, 95% CI 1.48-30.05, p = 0.004). Factors with adverse prognostic impact on PFS were: LDH ≥ 480 UL (HR: 4.47, 95% CI 1.42-13.73, p = 0.005), albumin < 3.5 g-dl (HR: 3.39, 95% CI 1.07-10.72, p = 0.007), hemoglobin < 100 gL (HR: 2.80, 95% CI 0.95-8.10, p = 0.048), platelets < 100 x 109 (HR: 2.78, 95% CI 0.95-8.02, p = 0.050), high-risk Arcaini score (HR: 7.32, 95% CI 1.96-27.34, p = 0.0007) and SMZL-Working Group high-risk score (HR: 7.29, 95% CI 2.25-23.56, p = 0.001). Despite the relatively low number of patients, no superiority was observed between the therapeutic regimens used, including rituximab monotherapy, splenectomy and low-intensity cytotoxic therapy, in relation to the outcomes 5 year-OS (p = 0.565) and PFS (p = 0.530) -Table 2. However, baseline characteristics differed between therapeutic groups in a statistically significant manner, and patients treated with rituximab or low-intensity cytotoxic therapy had a median LDH (p = 0.050) and B2 microglobulin (p = 0.048) higher than the group treated with splenectomy, as well as lower albumin value (p = 0.005), higher rate of comorbidities (p = 0.0002), worse performance status by ECOG (p = 0.050) and greater number of individuals with high-risk SMZL-Working Group score (p = 0.030) -Table 3, thus justifying the results described.
Conclusion: Therefore, in resource-poor settings, where access to anti-CD20 immunotherapy is not universal for patients with SMZL, we suggest that the first-line treatment should consist of monotherapy with rituximab for elderly patients, with high surgical risk or with at least one risk factor identified in our study. Remainders can be safely managed with splenectomy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal